2025 Annual Summary
Introduction
None of this would be possible without the commitment of clinicians, researchers, partners, and supporters across the world.
This year has been a period of meaningful growth for EECC Global. We generated more research than ever before, we implemented EECC in hundreds of health facilities, we produced face-to-face training materials, deepened partnerships across the world and massively increased our global network. Through workshops, champions, National Hubs, and steady communication with members, our clear and strong vision for how essential emergency and critical care can be delivered is spreading.
Dayana, a seven-month-old baby, was rushed to hospital after days of fever, vomiting, and worsening breathing. By the time she arrived, she was dangerously weak and struggling for every breath. A nurse trained in EECC immediately checked her vital signs and started oxygen therapy, calling for a doctor to assist. Tests confirmed pneumonia, and she was admitted for antibiotics and ongoing monitoring. Over the next week, her oxygen needs lessened, her breathing eased, and she grew stronger. Soon she was smiling and playful again, ready to return home.
Dayana’s story shows how EECC transforms a child’s near-fatal illness into recovery. Read more patient stories.
Major Research Published
This year saw the publication of several important studies that continue to build the scientific foundation for EECC.
African Critical Illness Outcomes Study (ACIOS)
Published in The Lancet, ACIOS is the most comprehensive description of critical illness in African hospitals.
Key findings include:
A high prevalence of critical illness: 12.5% (1 in 8) of adult inpatients in hospitals are critically ill.
Most care is on general wards: 69% of the critically ill are being treated in general wards rather than in specialized units
High mortality of critically ill patients: 21% of critically ill patients die in hospital within seven days, compared to just 2.7% of non-critically ill patients.
Lack of EECC: More than half of critically ill patients (56%) do not receive the low-cost and simple EECC they require, such as oxygen for respiratory failure and fluids for circulatory failure.
Realising the Benefit of Medical Oxygen
The Lancet Global Health Commission on Medical Oxygen Security reported this year, and included EECC. It provided a systems view of why hospitals struggle with reliable oxygen and described the importance of basic processes for oxygen safety and delivery. Key findings include:
60% of people continue to lack access to oxygen
82% of those in need (306 million) are in Low and Middle Income Countries, where coverage of oxygen is only 30%
The global need for oxygen is rising due to aging populations, lifestyle factors and air pollution.
Only 54% of LMIC hospitals have pulse oximeters, the simple equipment that identifies a patient’s need for oxygen
$6.8billion is required each year to provide oxygen to all, and that oxygen is a highly cost effective investment compared to other health related interventions, at just $59 per healthy life-year saved.
Published alongside the Commission’s report was an EECC commentary describing how to “realise the benefits of oxygen through essential emergency and critical care”. The key message is that oxygen will save lives when delivered as part of broader essential emergency and critical care. The commentary calls on governments, WHO, funders and professional societies to embed EECC into policies, guidelines and health benefit packages. The pandemic brought attention to oxygen, but without the wider EECC package its full impact cannot be realised.
Hospital Burden of Critical Illness across Global Settings
Published in BMJ Global Health, this study shows the scale of critical illness among admitted patients across diverse contexts. Key findings include:
Critical Illness prevalence is high: 12% (1 in 8) of patients in hospitals are critically ill.
Care is almost always on General Wards: 96% of the critically ill are being treated in general wards rather than in specialized units
Critically ill patients have a high mortality: 19% of critically ill patients die in hospital within 30 days (compared to 3% of those not critically ill)
The findings are consistent in high and low resource settings
Lessons learned from the promotion of Essential Emergency and Critical Care in Tanzania
This study described how Tanzania successfully promoted and integrated EECC into national policy. Drawing on interviews with policymakers, clinicians, researchers and implementation partners, the research identifies the practical lessons, strategies and enablers that supported EECC adoption across the health system. These insights offer valuable guidance for countries seeking to strengthen the care of critically ill patients. It is important to:
Work with the government early and consistently.
Use strong evidence to drive understanding and action.
Communicate clearly to correct misconceptions about EECC.
Use windows of opportunity, such as COVID-19, to advance EECC.
Embed EECC within existing health programmes.
Implement EECC through a multifaceted, system-wide approach.
Hospital Transport and Patient Deterioration Study
This study explores what happens when critically ill patients are moved between services or hospitals.
It showed that long delays, limited equipment, and poor communication contribute to deterioration during transport.
The findings highlight that the design and organisation of hospitals do not facilitate quick, short, and safe transport for critically ill patients, that hospitals lack the resources needed for safe and effective transportation and that there are weaknesses in the preparation for, conduct of, and handover of information concerning the transportation of critically ill patients
Together these publications reinforce a clear message. Many patients in low resource and high resource settings fall critically ill, often without reliable support. Simple and timely care can save lives, but only if hospitals are prepared and staff are equipped. Read more of our research.
At just four months old, Baby Deborah was rushed to hospital by her worried parents, struggling to breathe. A nurse trained in EECC immediately saw she was critically ill, with low oxygen and rapid breathing. She was taken to the resuscitation room, given oxygen, and positioned to ease her breathing. Gradually, her oxygen levels improved. Deborah was diagnosed with severe pneumonia and admitted for antibiotics and continued monitoring. Over the next four days, she grew stronger, her breathing normalised, and she was smiling again.
Her survival shows how EECC equips frontline staff to save babies’ lives with simple, timely care. Read more patient stories.
Implementation in Tanzania
The EECC in Tanzania programme (EECCiT) implemented EECC in >300 health facilities in five regions of mainland Tanzania and Zanzibar in 2025.
Preliminary findings after implementing EECC include:
Health workers successfully identifying and managing critically ill patients using EECC processes
Improvements in observation of vital signs, teamwork, and rapid responses
Positive engagement of regional, district and facility leaders that improves the availability and readiness of essential equipment and supplies
Increased coverage of EECC. More hypoxic patients receiving oxygen. More shocked patients receiving intravenous fluids. More unconscious patients having their airway protected.
Improved outcomes of critically ill patients.
Feedback from Implementers
Hospital Lead, Dr Stanford Ngeta, head of Vwawa District Hospital in Songwe Region, reports that the EECC programme has changed the way staff recognise and manage critical illness. He describes the earlier identification of danger signs, greater confidence among health workers, and faster responses when patients become unwell. He notes that staff now have a clearer understanding of what to do in emergencies and EECC has prevented avoidable deterioration in patients.
Regional Lead, Dr Jonathan Budega, Regional Medical Officer in Katavi Region, reflects on the wider improvements taking place across facilities. He highlights better hospital readiness, more consistent recognition of critical illness, and stronger supervision and follow up. He also reports reductions in maternal and newborn deaths linked to more reliable early care. Dr Budega describes this progress as something that has “never happened in history,” emphasising the scale of change underway.
Amina, 20, arrived at a district hospital in Tanzania bleeding heavily after a miscarriage. She was pale, weak, and in shock, with dangerously low blood pressure. A nurse trained in EECC quickly recognised her condition and called for help. Together, the team inserted an intravenous line, rapidly gave fluids, and raised her legs to keep blood flowing to her brain and vital organs. Within minutes, Amina’s strength began to return and her vital signs improved. After further treatment on the ward, she made a full recovery and returned home to her child.
Her story highlights how EECC saves mothers from preventable emergencies. Read more patient stories.
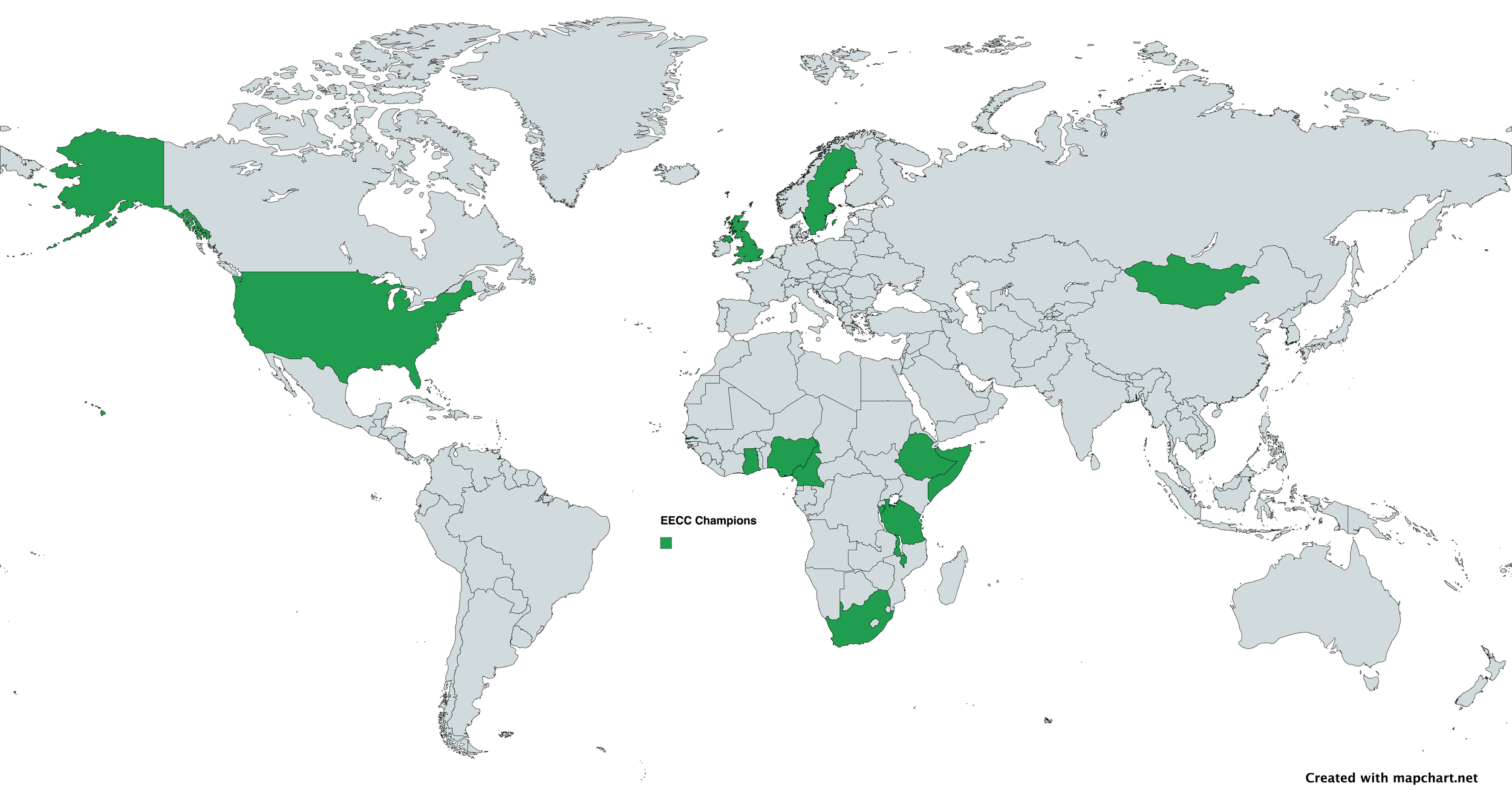
Champions Workshop
An EECC Champions Workshop was held in Dar es Salaam in May. This three day event brought together experienced clinicians, educators, and early adopters of EECC. Participants from Tanzania, South Africa, Ethiopia, Sweden, Malawi, Burundi, Gambia and Somalia explored issues around EECC, including the clinical processes and the hospital readiness requirements, practised ward based scenarios and discussed barriers to implementation in their own settings.
The workshop deepened understanding, strengthened advocacy skills, and supported participants to develop realistic action plans for their hospitals. By the end of the workshop all participants became EECC Champions and each left with a plan to strengthen early identification of critical illness, improve teamwork, support training in their facility, and raise awareness among colleagues.
EECC Global has now trained 116 EECC Champions. Read more.
Growth of National Hubs and Groups
There are now 10 EECC Global National Hubs promoting and implementing EECC in their countries.
In Malawi, the Hub is planning a national EECC assessment and has conducted a national training workshop in Lilongwe. A major training workshop, and is strengthening advocacy with hospital and government partners.
Malawi
Somalia
Facility assessments, training, and EECC online learning continue at Royal and Demartino Hospitals. The team is collaborating with the Somali ICU and Development Hub and strengthening links with Somaliland colleagues. Shared action plans and ongoing training are helping shape a national approach to integrating EECC across Somali hospitals
Burundi
The Burundi Hub is progressing with a national nurse mentor initiative. Recruitment and training of seven mentors are under way, alongside French translation of EECC materials and a December 2025 training-of-trainers programme. The Hub’s action plan guides assessments, mentorship, and early system-wide engagement across Burundi.
Nigeria
The Nigeria Hub has established a National Working Group and eight zonal teams. Current work includes baseline assessments using the EECC facility tool, delivery of standardised education sessions, and preparations for national conference participation. Nigeria is also supporting the formation of a West Africa Regional Group to expand EECC across the region.
Sweden
The Sweden Hub is advancing EECC through implementation research, training development, and international advocacy. Recent activities include a national network meeting, a Hub follow-up meeting, and preparations for a 2026 Champion Workshop. The team continues to coordinate EECC learning and outreach across regions, guided by Sweden’s 2025–2026 national agenda.
There are an additional 6 EECC Groups with 7 other countries pending - groups of motivated EECC practitioners looking to expand EECC activities in their countries. The Rwanda group, supported by the Rwanda Anesthetists Organisation, has held its first meeting and submitted a national proposal. Plans include assessments in six institutions, partnerships with NGOs and coordination with regional training initiatives. The Somaliland group is preparing for its first EECC training at Hargeisa Group Hospital. The emerging group is supported by the Somaliland Emergency Medicine Association and is building action plans and regional partnerships to sustain EECC activities.
South Africa
The South Africa Hub is advancing EECC through research, planning, readiness assessments and clinical training. The team is conducting research, drafting readiness assessment protocols for major obstetric units, and conducting simulation-based EECC workshops.
Ethiopia
The Ethiopia Hub has completed EECC assessments in 20 Addis Ababa hospitals and shared results with the Ministry of Health. Funding has been approved for national training and leadership workshops. The team is preparing for the All-African Emergency Care Conference and strengthening academic collaboration through trainee exchange activities.
Gambia
In The Gambia, national engagement is expanding through registration with the Ministry of Justice and outreach to hospitals and clinics. The team is rolling out VSDT charts, running workshops on recognising deterioration, and seeking accreditation with African and global critical care nursing bodies to strengthen EECC implementation nationwide.
United Kingdom
The UK Hub is strengthening EECC collaboration through partnerships with SAFE Anaesthesia, the IRC network, and specialist equipment providers. The team is supporting international training efforts by sourcing essential supplies, including low-cost airway manikins, and exploring funding opportunities through WFSA and other networks to advance EECC education and global implementation.
Tanzania
EECC work in Tanzania focused on strengthening implementation through the EECCiT programme. Activities included refining and delivering in person EECC training, supporting hospitals across multiple regions, conducting supervision visits, and sharing clinician feedback. These efforts improved readiness, early recognition of critical illness, and confidence among frontline health workers.
The Mauritania group has formed a diverse clinical team and met with the Minister of Health to request recognition and space for training. The group is preparing early activities while expanding membership and organisational capacity. The Nepal group is conducting a multi-hospital study assessing EECC readiness, availability of resources and workforce capacity.The Ghana group’s training at Komfo Anokye Teaching Hospital has led to new plans for structured handovers, basic triage and expansion to other hospitals. The team is integrating EECC thinking into ward routines and morning reporting.
Training and job aids
Training is a key aspect of EECC implementation. It gives health workers structured skills to identify and act early while also supporting communication and teamwork. EECC training has been strengthened through 2025 across multiple areas:
A 3-day face-to-face EECC course was developed and refined through delivery in Tanzania and is now available open access and free in complete form including facilitator manuals, pocket handbooks, slide decks, and evaluation materials
Health workers reported increased confidence, improved understanding of early warning signs, and a stronger sense of responsibility in emergencies
Multiple participants described how simulation, structured scenarios, and teamwork exercises improved real world performance
EECC Network Growth
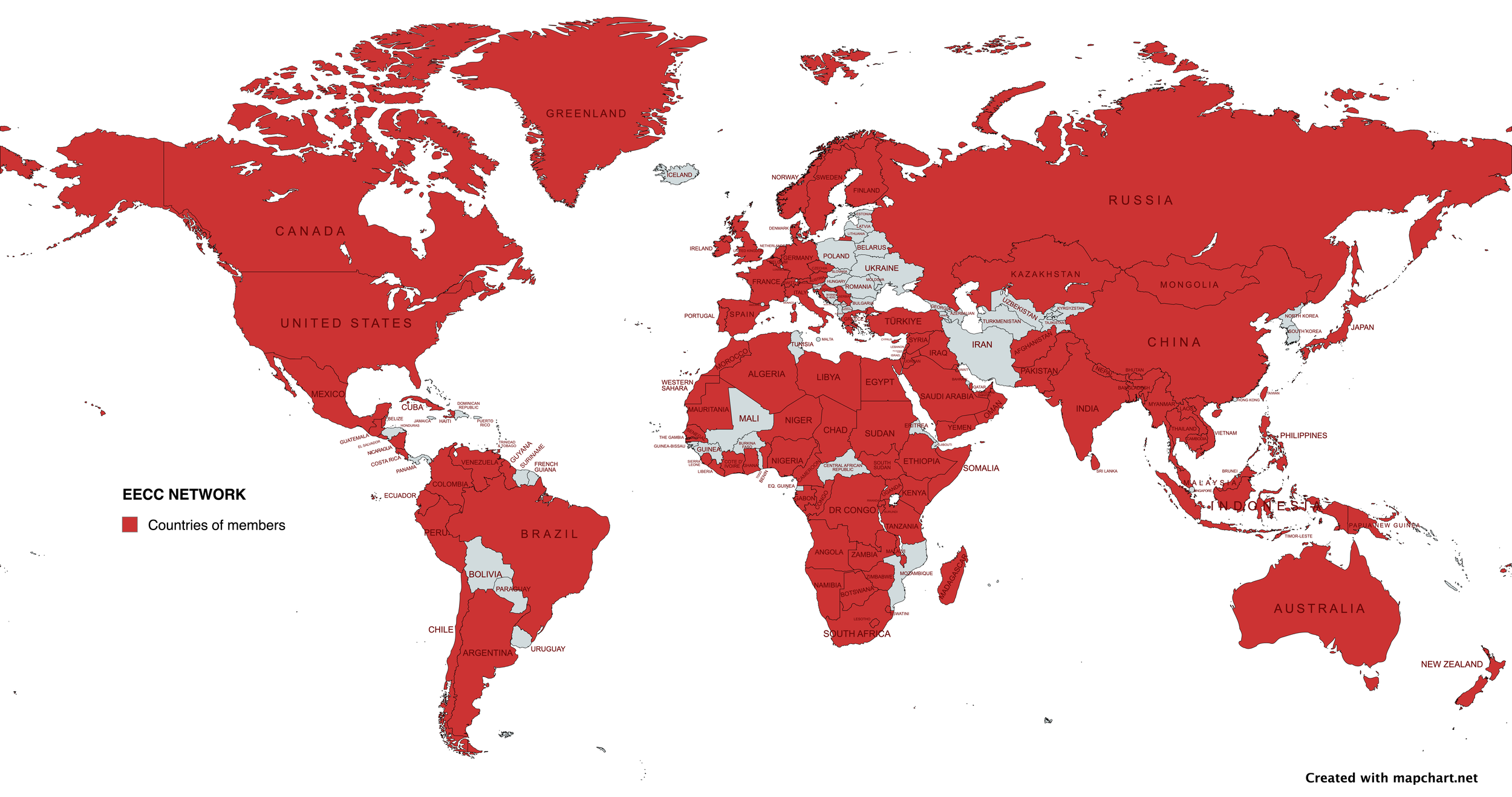
The EECC Network grew from 850 members in 96 countries at the start of the year to 1700 members in 127 countries at the end of the year. Join the EECC Network here.
Special Thanks
EECC Global wishes to thank the support of all our monthly donors and other funders who have made our work possible. A special thanks to Birgitta and Claes Eriksson, whose generation monthly donations have significantly enabled our work in 2025.. They commented:
“After many visits to several African countries, we have seen evidence that the work EECC does truly saves lives. Another important thing for us is that the money we donate does not disappear in bureaucracy”
Partnerships & Conferences
EECC Global has been working with and supporting many partners during 2025 including UNICEF, the World Bank, WHO, WFSA, WFICC, Laerdal Foundation, Medicins Sans Frontieres, Muhimbili University of Health and Allied Sciences, Karolinska Institutet, The Lancet Global Commission on Medical Oxygen Security, Every Breath Counts, InFACT and the Society of Anaesthesiologists in Tanzania.
EECC was presented and discussed at meetings and conferences including the World Congress of Intensive and Critical Care, the InFACT Global Meeting in Rwanda, Tanzania National Medical Congress, the Union World Conference on Lung Health, and the MUHAS Scientific Conference.
Fundraising
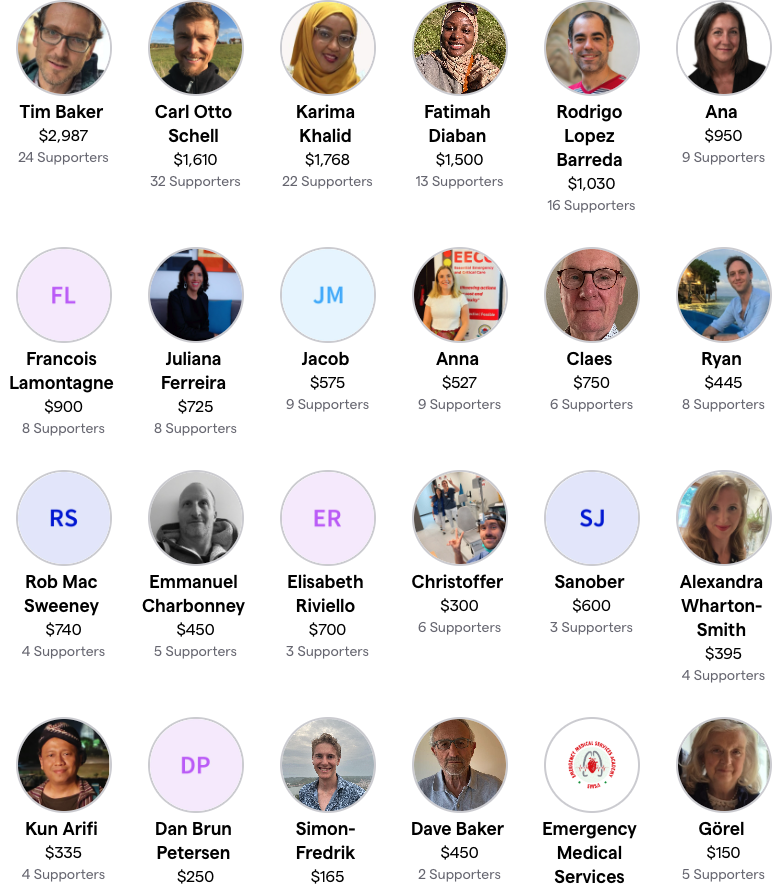
Thank you to the 100+ volunteers and 300 donors who helped us raise almost $25,000 in our ‘From Dayana to Thousands’ campaign in November and December
Thank you to our monthly donors whose ongoing contribution are vital to the backbone of our work.
And thank you to all of our one-off donors who have made a meaningful contribution towards increasing the provision of EECC.
You can make a donation here.