How Vital Signs Can Save Lives: The Power of Noticing Early Warning Signs
Every day, hospital staff make countless observations of patients: checking breathing, pulse, blood pressure, or oxygen levels. These measurements may seem routine — but they can be the difference between life and death.
When vital signs show that a patient is deteriorating, quick action can save them. Yet in too many hospitals around the world, these early warning signs are missed or not acted upon. The result? Preventable deaths.
Why vital signs matter
A patient becomes critically ill when their vital organs start to fail. This can happen with almost any condition — from infections like pneumonia, to trauma after an accident, to complications in childbirth.
The beauty of vital signs is that they give us an early, objective signal of trouble. A dangerously fast breathing rate, very low oxygen level, weak pulse or drop in blood pressure all indicate that urgent action is needed, no matter the underlying diagnosis.
In other words: you don’t need to know why someone is deteriorating to know they need help now.
Evidence from Tanzania: Vital Signs Directed Therapy
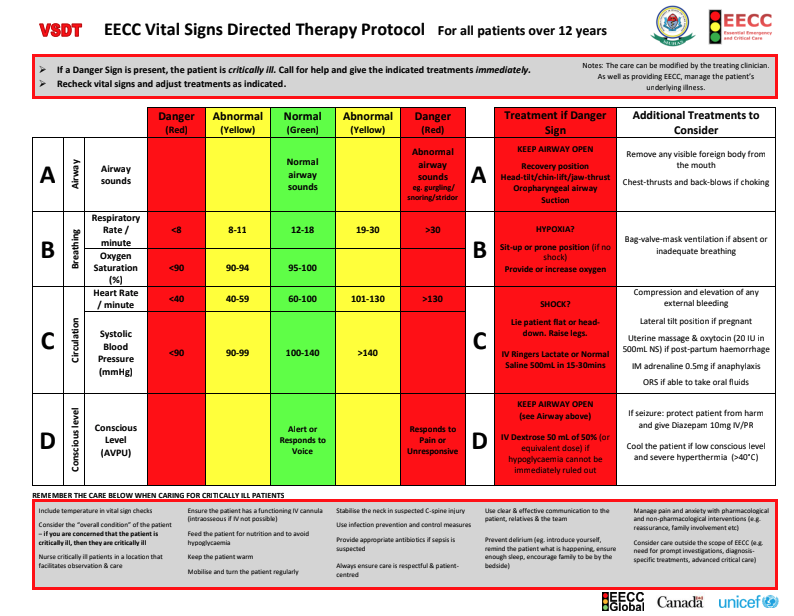
A study at Muhimbili National Hospital in Tanzania tested a simple protocol called Vital Signs Directed Therapy (VSDT).
Here’s how it worked:
Nurses and doctors measured patients’ vital signs.
If one was severely abnormal, they were prompted to take immediate action — for example, giving oxygen, IV fluids, or repositioning the patient’s airway.
The protocol was designed to be clear, fast, and feasible in a busy ICU with limited resources.
The results were dramatic for patients in shock. Survival increased from 8% before the protocol to 31% after its introduction. That means almost four times as many people survived a life-threatening emergency, thanks to timely action triggered by vital signs.
Moreover, a follow up study two years later showed adherence to the protocol had increased. Since many interventions decline post-study, this demonstrates a sustainable increase in the treatment of deranged vital signs.
Why warning signs are often missed
If vital signs are so powerful, why are they often ignored? Research from Schell’s thesis and beyond highlights several reasons:
Competing priorities: Staff are often focused on diagnosis and treatment plans, rather than urgent organ support.
System gaps: In some hospitals, vital signs aren’t routinely monitored, or equipment like pulse oximeters isn’t available.
Culture: In busy wards, abnormal results can be noted but not acted upon, because staff assume a doctor will review the patient later.
In the UK, for example, studies have shown that 75% of patients who had a cardiac arrest in hospital had clear warning signs beforehand — but those signs weren’t addressed.
The EECC approach: acting early, saving lives
This is where Essential Emergency and Critical Care (EECC) comes in. EECC is a package of 40 simple, life-saving actions that all hospitals should deliver. Monitoring and responding to vital signs is at the heart of it.
By making vital sign monitoring routine, ensuring staff are trained to act, and putting the right tools (like oxygen and fluids) within reach, hospitals everywhere can save lives — without the need for high-tech interventions.
The power of the basics
Vital signs are more than numbers on a chart. They are an early warning system, a chance to intervene before it’s too late.
The evidence is clear: when hospitals respond promptly to abnormal vital signs, patients survive. When they don’t, lives are lost unnecessarily.
At EECC Global, we believe that every patient deserves this basic level of care, no matter where they are. Because sometimes, the simplest measures are the most powerful.